Background
Along with my sisters, I cared for my mother through chronic and acute illnesses and during her dying process. After she died, I was the sole executor for her estate while going through the profound disorientation and grief of the loss. I felt upside down, inside out, and more often than not, isolated and overwhelmed. On the one-year anniversary of mom’s passing, my lifelong teacher and mentor told me her cancer was back. We spent the next 18 months exploring illness, life, and death on the phone, and I guided her through her final transition in person.
During these moments, I relied on my experience as a librarian to absorb and organize information quickly, on my facilitation and conflict mediation skills to listen deeply to the emotional content of a conversation in addition to the words themselves, and on my introspection and meditation to process and moderate my own emotional reactions.
It was a lot. Family members were not all on the same page. Everyone was doing their best, everyone was in pain, and things were not smooth.
While these are not the only losses I’ve has experienced, they were pivotal and led me to deepen my experiential understanding of life and death processes through formal study, psychotherapy, dream work, and community connection. Eventually, I earned an End-of-Life Doula certificate from the University of Vermont Osher Center for Integrative Medicine in 2024.
The Problem
It’s no secret that the U.S. healthcare system has gaps large enough to drive a planet through. Mainstream culture (think: movies, news, TV commercials, toys, music, and on and on) treats death as a curse or bogeyman, never to be discussed in polite company. On the historical view, the settler colonial project of white supremacy, capitalism, and misogyny have actively disconnected, suppressed, and destroyed customs that acknowledge death as a normal part of the life cycle. As a result, too many of us are under-resourced and unprepared for our own deaths and the deaths of those we love most.
Together, these big-picture processes shape the experience of individual people and families. By and large, people in the U.S. are left to fend for themselves when death approaches. The work of caregiving, appointments, financial and legal obligations, final wishes, emotional and spiritual counseling, and so much more end up on the shoulders of the people most affected by the death and loss. More often than not, the work disproportionately winds up with women in the family.
As a result, in the last stage of life, a dying person may spend long hours in isolation while their loved ones are too wrung-out to spend quality time together. After a death, people who’ve lost their loved one may feel disconnected, their relationships with each other fraught, with no central place or practice to guide them through their normal and healthy experience of grief. Sorting through the legal and financial steps after death may feel like navigating a thorn-filled labyrinth in pitch darkness with floors that pour salt on fresh wounds.
Approaches to Solutions
Thank goodness I’m not the first person to notice these problems and want to do something about it!
In recent history (i.e., since the 20th century), the hospice movement has made great strides in re-humanizing people who are dying in the Western world.
Going a step further, end-of-life doulas (“death doulas”, “death midwives”) have begun reintegrating end-of-life care within the context of a person’s regular life and family. They nurture, inform, support, guide, empower and comfort people preparing for or experiencing end of life.
What I provide
My approach considers a person who is dying and their loved ones as whole organisms in a living ecosystem with multiple levels of experience.
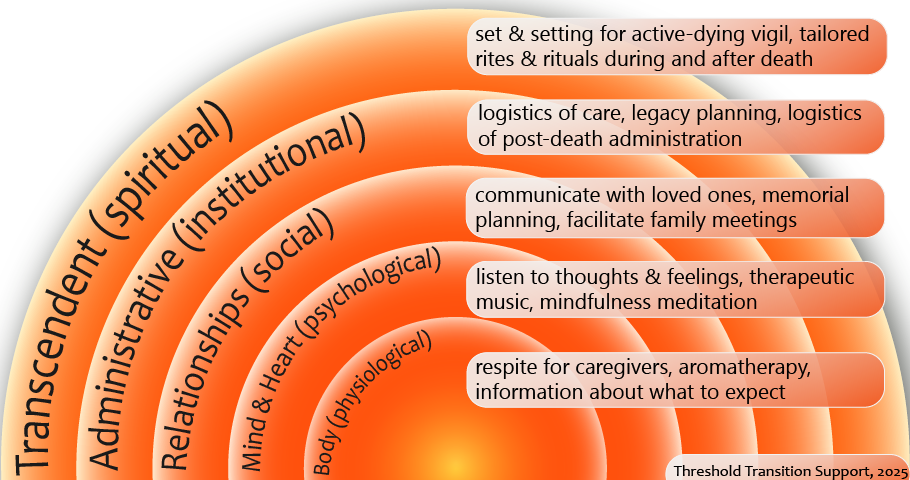
I made the above diagram to summarize the domains of work I can support and am repeating the text here so that people using screen readers can access the information.
- The Body (physiological level)
- offerings: respite for caregivers, aromatherapy, information about what to expect, easy-to-understand education about the biological processes at work
- Mind & Heart (psychological level)
- offerings: listen to the thoughts and feelings of a dying person and their loved ones, tease out personal and organizational needs, provide therapeutic music (live or recorded), practice and guide mindfulness meditation
- Relationships (social level)
- offerings: support informing loved ones of a person’s illness or death, facilitate family meetings, support identifying roles & responsibilities
- Administrative (institutional level)
- offerings: coordinate logistics of care; legacy planning; documenting personal, emotional, medical and spiritual wishes during and after death; logistics of post-death administration
- Transcendent (spiritual level)
- offerings: guide vigil during active dying stage, facilitating rites and rituals tailored to your beliefs
You may only need help with one or two areas or a full spread – there is no obligation to engage with any particular offering.
Fees
Individuals & Families
Full Rate
Sliding Scale
Hourly Rate
$175.00
$125.00
Package of 5 hours
$825.00
$525.00
It’s important that we get to know each other before committing to intense work, so I provide a 1-hour consultation at no charge. If you need last rites performed urgently and can’t afford the discounted rate, please reach out anyway and I will do my best to accommodate.
How to get in touch
You can book a free consult with me now, fill in the brief form on the contact page of this website, email me at change@thresholdsupport.org, or call or text me at (815) 270-5972. I look forward to hearing from you.

